Medical device development is one of the most complex manufacturing processes associated with stringent requirements and quality standards. The development cycle for any medical product involves several unique stages to ensure effective and safe production. The stages range from concept development to medical product design, prototyping, testing, verification & validation, and mass production.
Although the exact medical device product development process differs from region to region. Different regions also have their standard regulatory requirements. However, the phases and their requirements have several similarities across the board.
This guide will focus on the key stages of the medical device development process, touching on the development timeline for different medical products. We will also discuss the various challenges and opportunities for product development in the medical device industry.
Key Stages of Medical Device Development and Typical Timeline
Medical devices are expected to be designed and manufactured with utmost precision and care. These products must meet the various requirements for their intended uses. Therefore, essential stages need to be followed in the medical device development lifecycle.
Stage 1: Ideation, Conceptualization, and Risk Analysis (1-2 months)

The initial stage of the medical device development process involves meticulous planning, extensive research, and thorough documentation. It is important to consider opportunity and risk analysis to make this process more distinctive. Conducting a risk analysis is crucial to determine whether progress can be made in subsequent phases.
Creating a medical device is a challenging endeavor that necessitates careful consideration of your requirements. This data will inform your risk analysis. It is vital to establish a comprehensive development plan for your medical device. Typically, a medical product design and development plan encompasses the following sequential steps:
- Clearly define the intended use of the medical device.
- Identify existing similar or equivalent products already available in the market.
- Evaluate consumer demands and establish differentiating factors for your proposed product, ensuring its viability.
- Gather user needs to serve as inputs during the design process.
- Analyze how users would typically interact with the product, whether it’s an existing device or one that will be invented.
Importance of Ideation and Risk Analysis
It is essential to devise funding strategies and carefully select the target markets during the first phase of medical device development. Questions like where to enter the market, why, and how should be thoroughly analyzed. The risk and benefit analysis must be continually updated throughout development and even after launching the device.
Detail why and how the new device will benefit users and outline any potential risks it may pose. This step is crucial due to the diverse regulations and challenges inherent in different markets. If you are developing a novel product, be sure to safeguard your intellectual property by considering patent protection.
Market research is a fundamental component in this initial medical device product development phase. It will help determine if similar devices on the market can be used as precedents or if there is a need for clinical trials. The distinction between the two approaches can significantly impact the feasibility of your venture due to the associated costs. Thoroughly document the outcomes of your market research.
Stage 2: Formulation, Regulatory Compliance (6-12 months)

During the second phase, conducting a formal risk assessment and gathering regulatory and customer requirements becomes crucial. This is an opportune moment to proactively address risks and consider your customers’ needs. The customer’s perspective holds significant value, so it is important to actively seek feedback through surveys and interviews. Utilize these valuable insights, along with market research and competitor analysis, to integrate them into the design of your product.
Regulations and Quality Management System
It is crucial to clearly understand the regulatory requirements applicable to your device. FDA regulations and guidelines must be followed for every medical device. It would be best to also take note of the specific regulatory and safety requirements of the country or region in which you intend to sell.
Implementing a quality management system (QMS) is another vital step during the first phase of medical device development. Your QMS serves as the cornerstone of your company and, once established, provides a solid foundation upon which to build. ISO 13485:2016 is a widely adopted international standard with significant recognition in the medical device industry.
Your QMS should encompass a comprehensive set of procedures, forms, templates, and standard operating procedures (SOPs). These ensure that all aspects of your medical device development and manufacturing processes are tightly controlled and monitored.
Stage 3: Design Development, Verification, and Validation (6-12 months)
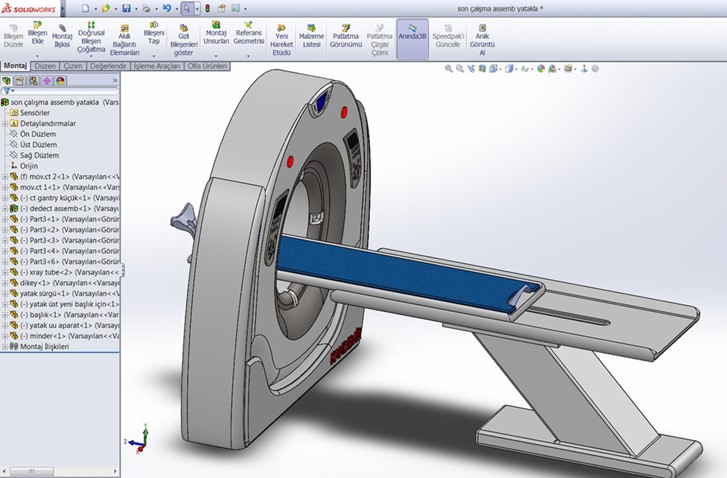
Having achieved proof of concept, the subsequent phase revolves around controlling the generation of design inputs and design outputs. The medical device design requirements encompass various elements, including product drawings, bill of materials (BOM), specifications, work instructions, and more.
The third phase of medical device product development places significant emphasis on validating and verifying your design. Throughout this stage, you must follow a continuous planning, design, review, and approval process. This approach creates an auditable trail demonstrating the steps taken to mitigate risks of failure and potential harm to end users.
Engineering requirements play a pivotal role in addressing essential questions, such as:
- How will you fulfill customer requirements?
- What testing methods will you employ for verification and validation?
- What processes are necessary?
- What test equipment will be required?
- Have you considered a manufacturing and quality plan, or will you opt for outsourcing?
Importance of Design Development Stage
This phase also presents an opportunity to leverage your risk management practices. Document all potential failure modes resulting from design flaws, inadequate manufacturing processes, or foreseeable user errors. A comprehensive assessment of potential risks is vital, as failure to address safety concerns may prevent your device from reaching the market.
Additionally, it is essential to update your regulatory strategy as needed. If you previously determined that clinical trials are necessary for your product, you should initiate your clinical investigation. Furthermore, consider the external approvals required to align with regulatory requirements.
Stage 4: Manufacturing and Testing (6-12 months)

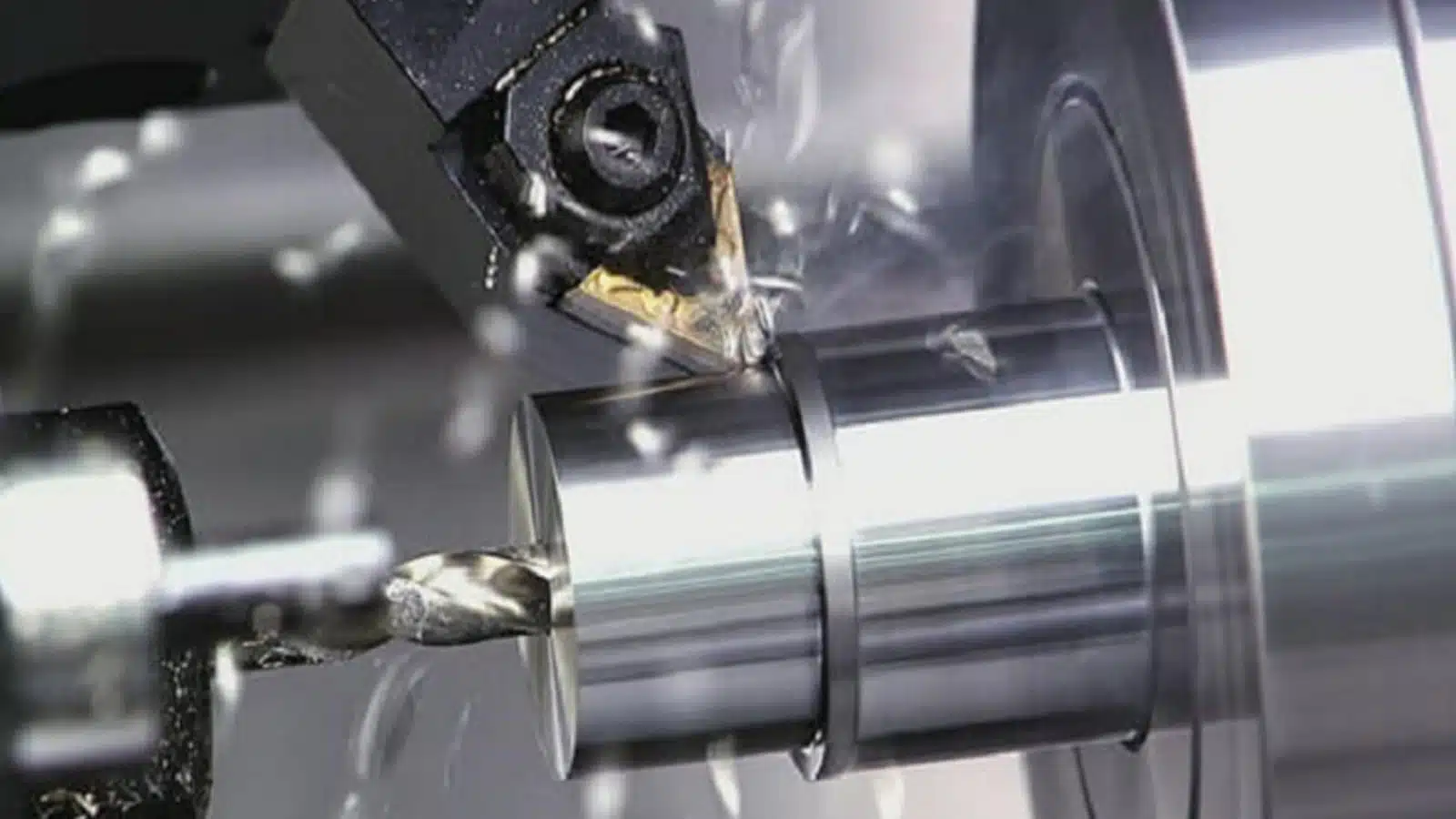
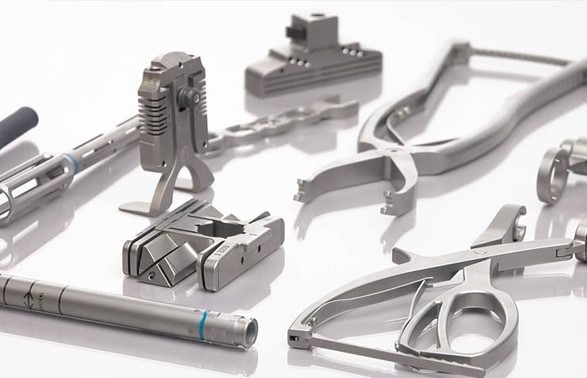
The focus shifts towards manufacturing and testing in the fourth stage of medical device development. This stage requires a coordinated effort among cross-functional teams, including engineers, manufacturing personnel, quality assurance experts, and regulatory specialists. It encompasses several critical aspects ranging from design for manufacturability (DFM) to quality assurance.
Optimizing the design of the medical device to ensure smooth and efficient production. Thus, DFM aims to simplify manufacturing processes, enhance productivity, reduce costs, and minimize potential manufacturing issues. Considering DFM principles during the design phase, you can streamline the transition from prototype to mass production.
Furthermore, careful consideration is given to selecting materials that possess the necessary properties and comply with regulatory standards. Sourcing reliable suppliers and establishing a robust supply chain is crucial to ensure consistent material quality and availability.
Choosing the Right Manufacturing Process
Determining the most suitable manufacturing processes and techniques involves selecting the appropriate methods for fabricating, assembling, and finishing the device components. Depending on the complexity and nature of the device processes such as injection molding, machining, extrusion, casting, or additive manufacturing may be employed. It is crucial to evaluate the capabilities and limitations of each process to ensure efficient and accurate production.
Maintaining stringent quality control and assurance procedures throughout manufacturing is paramount to delivering safe and reliable medical devices. This involves implementing quality management systems, performing regular inspections and audits, and adhering to relevant standards and regulations. Quality control measures encompass testing and inspection of materials, in-process monitoring, and final product validation.
RapidDirect’s rapid prototyping service for medical devices encompasses these crucial aspects to ensure compliance with design specifications, functionality, and safety requirements.
Stage 5: Clinical Trials and Approval (1-3 years)

Once your medical device has reached a stage where individuals can safely use it, the next crucial step involves obtaining approval from the Food and Drug Administration (FDA). Before marketing the device for sale, it is necessary to notify the FDA. The approval process varies depending on the device’s risk level. Class III devices represent the highest risk, requiring clinical trials before going for PMA (Premarket Approval). While a small percentage of Class II devices may also necessitate clinical trials, it is not mandatory for all of them.
The pathway for starting clinical trials of medical devices is the IDE (Investigational Device Exemption). The FDA has the authority to approve the IDE, disapprove it, or approve it with certain conditions. In cases where the IDE is disapproved, the trials cannot commence until the identified deficiencies are addressed and the revised information is submitted for FDA review. Successful completion of clinical trials with positive data allows a company to proceed to the PMA application stage.
The primary objective here is to demonstrate that the new medical device is effective and safe for its proposed use. It also shows that the quality management system can maintain its safety and effectiveness. Furthermore, the FDA conducts inspections of the manufacturing facility responsible for producing the product to ensure adherence to GMP (Good Manufacturing Practices).
Stage 6: Launch and Post-Market Activities (Ongoing)

Once the FDA clears your product(s) and Quality Management System (QMS), you are ready to enter the market with your product(s). To ensure a successful launch, it is essential to have a validated and verified production plan that guarantees timely delivery, adherence to budget, and, most importantly, the production of safe and high-quality medical devices.
It is crucial to continuously verify that your plan aligns with regulatory requirements. Regular inspections, audits, and spot-checking should be conducted throughout your production and QMS processes. These measures serve as effective means to identify and address issues stemming from batch-to-batch variations.
Once your products are on the market, it is vital to gather data from various stakeholders, including users, patients, hospitals, technical operators, distributors, etc. Regularly analyzing this data is an integral part of the risk management process. Activities such as Post-Market Clinical Follow-Up (PMCF) and Post-Market Surveillance (PMS) ensure the ongoing safety, performance, and durability of the product.
Various documents and guides must be provided to assist users. These documents include Instructions for Use (IFUs), user training manuals, user guides, and commercial brochures. These documents must be created following relevant guidelines and regulatory requirements. It is important to note that the necessity for these documents may vary depending on the classification of the device. Therefore, confirming the specific requirements applicable to your device classification is crucial.
By prioritizing post-market data collection and maintaining compliance with regulatory obligations, you can ensure product safety and quality.
Accelerate Your Medical Device Development with RapidDirect
Are you tired of delays and inefficiencies in your medical device development process? Look no further! RapidDirect is your ultimate partner in accelerating your path to success.
With our unrivaled expertise and cutting-edge manufacturing capabilities, we empower you to navigate the complex landscape of medical device development with ease.
Development Timeline of Different Devices
The process of developing and obtaining approval for a new medical device can span several months or even years, depending on the nature of the device. The FDA’s approval ensures the safety and efficacy of medical devices before they reach the market.

The FDA provides guidelines for the time required to gain approval for different classes of devices to enter the market:
Class 1 Devices
These devices are considered low-risk and can be swiftly approved by the FDA. They include tongue depressors, oxygen masks, electric toothbrushes, etc. The majority of non-invasive Class 1 devices can be self-registered with the FDA. This process can be completed in as little as one week.
Class 2 Devices
Class 2 devices pose a moderate risk. They include items like contact lenses, catheters, and syringes. Approximately 43% of devices fall into this category. Manufacturers must demonstrate the safety and efficacy of their device by comparing it to another FDA-approved device. While the FDA provides a submission receipt within 60 days, the average clearance time is 177 days (around six months).
However, the clearance duration can vary depending on the specific type of device submitted. For example, anesthesiology devices have the longest average approval time, at 245 days. On the other hand, toxicology devices have the shortest time of about 163 days.
Class 3 Devices
Class 3 devices are the most invasive and carry the highest risk to patients. They account for approximately 10% of medical devices, including cochlear implants, defibrillators, and implanted prostheses. Due to the increased risk, these devices undergo the most rigorous scrutiny during the development process to obtain FDA approval.
The FDA requires substantial scientific evidence demonstrating the safety and efficacy of these products. On average, approval for Class 3 devices takes around 243 days (about eight months) after submission. Note that this waiting period has significantly reduced in recent years.
Challenges and Opportunities in Medical Device Development
Medical device manufacturers encounter various challenges, including quality issues, regulatory compliance, supply chain complexities, optimizing collaborative processes, etc. These factors pose significant hurdles that require careful consideration to ensure consumer safety and stakeholder satisfaction.
Some of these challenges include:
Costs and Funding Constraints
Developing a medical device involves significant research and development expenses. Costs can arise from conducting feasibility studies, prototyping, testing, and obtaining regulatory approvals. Moving from prototype to mass production involves additional costs. Manufacturing medical devices at scale require investments in specialized equipment, facilities, quality control systems, and skilled labor.
Despite these, securing funding for medical device production can be a major obstacle, especially for startups and smaller companies. This may significantly impede progress and hinder the development of innovative medical devices. Careful financial planning, cost optimization strategies, and efficient project management can help mitigate some financial burdens associated with medical device product development.
Regulatory Complexities and Evolving Requirements
Medical devices are subject to strict regulatory frameworks imposed by regulatory bodies. Some major regulations include ISO 13485, ISO 14971, 21 CFR 820, and MDR. Compliance with complex and evolving regulations is a significant challenge for device developers.
Moreover, regulatory bodies frequently update guidelines, standards, and submission requirements. This is a bid to adapt to technological advancements, safety concerns, and changing market dynamics. Staying updated with these changes and ensuring compliance can be demanding, especially for several years of long development cycles.
Manufacturers have a valuable opportunity to optimize their operations and enhance data management practices. This proactive approach fosters efficiency and empowers them to respond effectively during critical situations. By prioritizing seamless coordination and comprehensive risk management, stakeholders can collectively ensure the highest quality, safety, and compliance standards.
Talent and Expertise Shortages
The shortage of talent and expertise encompasses various areas, including skilled engineers, researchers, regulatory professionals, etc. The scarcity of such professionals can hinder the timely and efficient development of innovative medical devices. Lack of talent and expertise can lead to delays in product development, as finding qualified individuals with the necessary knowledge and experience may take time.
It can also result in suboptimal design choices, regulatory compliance issues, and reduced overall product quality. Furthermore, the fast-paced nature of technological advancements in the medical field requires a constant influx of fresh talent and expertise to keep up with the latest developments. Medical device manufacturers can invest in training and development programs to nurture their existing workforce and enhance their skills.
Emerging Technologies and Changing Market Dynamics
The fast-paced evolution of emerging technologies, such as artificial intelligence, the Internet of Things (IoT), and nanotechnology, presents challenges in keeping up with the latest developments. With new technologies comes the need for updated regulatory frameworks. Adhering to evolving regulations and standards can be challenging. It requires continuous monitoring and adaptation to ensure compliance while bringing innovative products to market.
Moreover, medical devices are becoming more interconnected and part of larger healthcare ecosystems. Ensuring seamless integration and interoperability between devices, healthcare systems, and electronic health records becomes a challenge. Therefore, it is important to harness the opportunities these emerging technologies offer to drive growth in medical manufacturing.
Future Trends and Opportunities of Medical Device Product Development
Innovative medical device trends focus on risk reduction, health data utilization, and process automation. Manufacturers employ various technologies and processes to enhance efficiency, productivity, and affordability.

Advanced Materials and Manufacturing Process
There is significant promise for medical device development regarding materials and manufacturing processes. Nanotechnology allows the manipulation of materials at the nanoscale, enabling the development of advanced medical-grade plastics with unique properties. Nanomaterials offer increased strength, improved biocompatibility, enhanced drug delivery capabilities, and better electrical conductivity.
Nanotechnology combined with additive manufacturing techniques allows the fabrication of complex medical devices with precise structures and customized designs. 3D printing at the nanoscale level enables the production of patient-specific implants, scaffolds for tissue engineering, and microfluidic devices with intricate geometries. This technology offers greater design flexibility, faster prototyping, and cost-effective production. Other technologies like medical injection molding are also receiving increased recognition.
Personalized Medicine and Precision Therapies
The concept of personalized medicine has grown substantially over the past years, revolutionizing the treatment landscape for numerous diseases. This ongoing progress is set to accelerate further with breakthroughs in genomics. It will empower healthcare professionals with deeper insights into the fundamental origins of illnesses and facilitate customized therapeutic interventions.
Medical products are becoming more sophisticated in analyzing individual patient data, such as genetic information, biomarkers, and other relevant parameters. This enables precise disease diagnosis and tailored treatment plans. This approach minimizes the potential side effects of traditional systemic treatments and enhances therapeutic outcomes.
AI and Machine Learning
The influence of artificial intelligence and machine learning has expanded the possibilities for ensuring high-quality patient care. One prominent trend is the application of AI and ML algorithms in medical imaging devices. These technologies can analyze medical images, such as X-rays, CT scans, and MRIs, to aid in detecting and diagnosing diseases.
Another area of opportunity lies in remote patient monitoring and wearable devices. AI and ML algorithms can process real-time patient data collected by wearable devices to monitor vital signs, detect anomalies, and provide personalized insights. This can enable early intervention, continuous monitoring, and improved disease management.
Regulatory Changes
There is an increasing emphasis on regulatory harmonization and global alignment. Regulatory agencies around the world are working towards aligning their requirements and standards. They aim to reduce duplication of efforts and facilitate global market access to medical devices. This trend allows manufacturers to navigate regulatory processes more efficiently and expand their reach to international markets.
Additionally, regulatory authorities are placing increased importance on monitoring medical devices’ performance, safety, and effectiveness once they are on the market. This allows manufacturers to collect and analyze real-world data, engage in active surveillance, and continuously improve their products based on post-market feedback.
Globalization and Expanding Markets
Countries with developing healthcare systems are experiencing an increased need for advanced medical technologies to address their evolving healthcare challenges. This opens up new market opportunities for manufacturers who can adapt their products to meet the specific needs of these regions.
Moreover, advancements in communication, transportation, and supply chain management have facilitated the expansion of markets and the distribution of medical devices across borders. Manufacturers can leverage these advancements to establish partnerships and collaborations in new markets.
Quick Question: Is FDA Approval Required for Medical Devices?
Yes, FDA approval is generally required for medical devices. The FDA regulates medical devices to ensure their safety and effectiveness before marketing and sales. The level of FDA oversight and the specific approval pathway depends on the risk classification of the device.
Class I and II devices typically go through a premarket notification process, also known as 510(k) clearance. Here, the manufacturer demonstrates that the device is substantially equivalent to a legally marketed device. This process does not involve full FDA approval but rather a determination of substantial equivalence.
Class III devices are considered high-risk or life-sustaining. They usually require a premarket approval (PMA) application. The PMA process involves a more comprehensive review by the FDA, including evidence of safety and effectiveness through clinical data.
In some cases, certain low-risk devices may be exempt from FDA premarket review. However, they still need to meet other regulatory requirements, such as adherence to quality systems regulations and compliance with labeling and manufacturing standards.
Conclusion
The medical device product development process can be complex, comprising various guidelines based on specific markets. You need to carry out adequate research and go through rigorous processes of ideation, designing, development, documentation, regulation, and more. We have outlined the processes involved in each stage of development. It is essential to follow each step while complying with regulatory requirements holistically.
At RapidDirect, our comprehensive medical device prototyping and manufacturing solutions will accelerate your product development efforts. We are ISO 13485:2016 certified, showing that we implement a strict quality management system to ensure the quality and safety of your medical device. We boast experienced technicians that will expertly bring your products to market within the shortest timeframe. Submit your design file today, and get an instant quote.